
08 Jun Analgesia and the gastrointestinal tract
Analgesia and the gastrointestinal tract – the hidden whole person impairment
By Dr Anthony Greenberg, Gastrointestinal & Trauma Surgeon
Personal injury lawyers are largely unaware of the effects of medication-induced gastrointestinal problems stemming from physical injuries. It is important that lawyers are made aware of these side effects, and are able to ask the right questions of their injured clients to help unearth any hidden gastrointestinal issues that may affect their compensation.
As a trauma and gastrointestinal surgeon, I have observed in my clinical practice that people who are injured not only have to endure the consequences of their injuries, but the treatments [medication] we give them can conversely make their situation much worse.
Work-related injuries, motor vehicle accidents and the like are often life-altering events that stop people from working and have a huge impact on their personal responsibilities and quality of life. The impact of chronic pain is a serious and ongoing problem for the injured person and also has a major impact on the family members and friends.
Injury manifests as chronic pain and also as mood change and mental illness which further complicates the situation. Injured people need analgesia to reduce the ravages of chronic pain to function at work and live a full and happy life.
Injured people often find themselves lost in the system and disabled following an injury that leads to major change in their life and loss of their ability to earn and provide. Obviously adequate pain relief is very important and fortunately very effective in the majority of cases.
 However, most medications are never a ‘silver bullet’ and are recognised to have side effects (adverse events.) Some side effects can be dangerous and others debilitating. This is particularly so with the gastrointestinal tract where the side effects of medications — although very effective — can be worse than the primary aim.
However, most medications are never a ‘silver bullet’ and are recognised to have side effects (adverse events.) Some side effects can be dangerous and others debilitating. This is particularly so with the gastrointestinal tract where the side effects of medications — although very effective — can be worse than the primary aim.
The mains groups of medications used for pain relief are:
- Non-steroidal anti-inflammatory drugs
- Opioids
- Medications used for neuropathic (nerve-induced) pain
- Antidepressants
- Benzodiazepines
I will concentrate on the gastrointestinal tract and the adverse events that are recognised to occur when patients are prescribed these medications.
Common adverse events due to medication
- Gastro-oesophageal reflux disease
- Analgesic gastritis
- Disturbance to the gastrointestinal motility (medication-induced gastrointestinal motility disorder)
Recognisable symptoms
These clinical conditions are manifested with recognisable clinical symptoms and findings on examination. Patients often report symptoms such as:
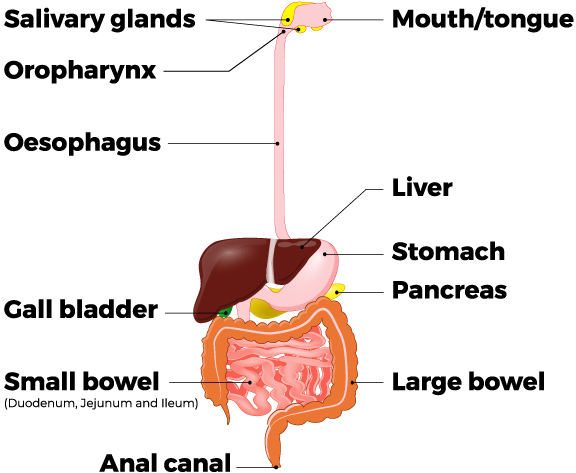
A ‘burning, acid-like’ sensation in their chest and throat. The reflux comes up behind the chest bone into the neck and up into their mouth (oropharynx). They often complain that their mouth is very dry. Nausea is very common and on occasions patients report they need to throw up.
Patients with reflux often describe their food gets ‘stuck’ in their neck or chest (dysphagia). The reflux often wakes people several times at night and is a very disturbing symptom. Patients wake up feeling short of breath when the acid reflux spills over into their laryingo-pharynx and irritates the vocal cords, causing a symptom where patients describe a feeling that they are suffocating. This is called reflux with overflow.
Many patients describe bad breath despite cleaning their teeth and using mouth washes. A very common complaint is that patients cannot eat a diet that they used to as it tends to trigger the reflux symptoms and they can only eat bland foods.
Lower gastrointestinal tract
On average, most people open their bowels once a day. Clearly this is variable and there is a normal distribution with some people opening their bowels every day while others may open their bowels every three to four days. All of these people fall into the normal distribution.
However, patients who require medication may have major changes in their bowel function, become very constipated and find their pattern changes. Constipation is not a harmless condition and is often associated with a lot of unpleasant and challenging symptoms.
People who used to open their bowels every day find they cannot go to the bathroom as they used to prior to taking medication. This can vary between every second day or once a week or sometimes even longer.
Far more than is commonly recognised, patients describe a number of effects that can have a major impact on their ability to work and their personal life. They often describe:
- Altered stools varying in size from small pebbles to large bulky hard stools that are very difficult to evacuate
- Needing to strain, push hard, getting pain around the anus and rectal bleeding
- Developing haemorrhoids, often due to all the straining
- Feeling bloated, distended, full and their abdomen tender to touch
- Excessive straining that compounds their spinal injury
- Embarrassing and offensive flatulence
- Cramping, abdominal pain, explosive diarrhoea, and needing to rush to the bathroom (urgency)
It is not uncommon for patients to be in the bathroom for long periods — 30 minutes or longer each time — with a feeling of never evacuating their bowel properly. We call this incomplete evacuation. On occasions they need to be in the bathroom several times a day, and each time for half an hour or longer.
Investigations
The main clinicians who are involved with patient care are:
- General Practitioner
- Gastrointestinal surgeon or medical gastroenterologist
- Pain specialist
Of the various investigations, the most important is the ability to inspect the alimentary tract by using fibreoptic endoscopy as part of either a gastroscopy and/or a colonoscopy. Gastroscopy and colonoscopy are used to exclude any underlying organic disease such as malignancy or peptic ulceration, and are the most important investigations used for gastrointestinal symptoms.
Gastrointestinal endoscopy is combined with imaging, such as CT and ultrasound scans or, less commonly, MRI scans to exclude any unexpected pathology. It is important that personal injury lawyers should look out for these symptoms as they are often not recognised without asking. It has been my experience that patients often will not report the gastrointestinal symptoms unless asked.
Many patients are not aware that the symptoms are medication-related or they may feel too embarrassed to talk about it. Patient suffering is therefore often not apparent unless looked for. As stated earlier, I have noticed on many occasions that the combination of the primary injury and the gastrointestinal side effects compound the original injury and make the situation worse.
These symptoms have a major impact on the patient’s:
- Quality of life
- Ability to work
- Family life
- Mental health
- Self-esteem
The questions that personal injury lawyers could be asking of their clients to uncover any hidden gastrointestinal issues are:
- What medications have you been prescribed?
- Are the medications for pain relief, neuropathic pain (referred or nerve pain), mood disorders (antidepressants) or any others?
- How long have you been taking these medications and who is prescribing them?
- Are you experiencing any side effects?
- Reflux
- Change in bowl function (constipation or diarrhoea)
- Vomiting
- Nausea
- What impact are the side effects having on your ability to perform your role at work and/or at home?
Conclusion
The gastrointestinal symptoms cannot be seen in isolation. It is recognised that these medications can cause significant adverse gastrointestinal events. The adverse gastrointestinal symptoms in combination with the physical injuries often affect a patient’s psyche and have a significant impact that sets up a cycle where everything can be interrelated and very difficult to break.
Armed with a heightened awareness of potential medication-induced gastrointestinal problems stemming from physical injuries, key questions to ask when onboarding a new client or review a case and the expert opinion of a gastrointestinal surgeon, solicitors can be of great assistance to improving their clients life, work and health outcome.
Further details
If your firm is keen to learn more about this topic, Dr Greenberg would be happy to perform an in-house presentation. For bookings, please email Darryn Midson from the ASSESS Medical Group at darryn.midson@assessmedicalgroup.com.au
Dr Anthony Greenberg is a General Surgeon with extensive experience in gastrointestinal surgery, trauma, and maxillofacial injuries. He has special expertise in the management of gastric conditions, including peptic ulcer and reflux disease; colorectal surgery, including haemorrhoids and bowel disease; and abdominal wall surgery including inguinal and femoral hernias.


